Immediately after the event, people often experience shock and denial. Longer-term reactions include mood swings, anxiety, flashbacks, nightmares, hypervigilance, strained relationships, and even physical symptoms such as headaches or nausea. While these feelings are normal, some people have difficulty moving on with their lives. As a result, trauma is considered a major risk factor in the development of not only post-traumatic stress disorder (PTSD), but also a range of other mental health conditions.
Trauma activates the instinctive survival reflex known as the fight, flight or freeze response; the physiological and psychological reaction to a danger or perceived danger. The autonomic nervous system floods the body with adrenaline and noradrenaline leading to rapid heart rate and breathing, tense muscles, nausea, sweaty palms, dilated pupils, racing thoughts or dizziness. It is priming the body to fight or flee the danger. While this state of arousal can in some situations increase our performance, a prolonged or persistent state of arousal is often associated with the development of acute stress disorder, anxiety, and even PTSD.
Bessel van der Kolk in his book The Body Keeps the Score (1996), details the impact of this prolonged state of arousal on the body and the brain, particularly memory. Traumatic events are not processed to memory in the same way as other life events. Trauma continues to intrude often via sensory triggers. These triggers may be a sound (a car backfiring being misinterpreted as a gunshot), a sight (a news bulletin showing familiar scenes), a smell (an open fire recalling a bushfire) or just a sensation of being followed. Traumatic event triggers activate and maintain the state of arousal. As van de Kolk says “your body keeps reacting as if you are still in imminent danger”.
PTSD is the disorder most commonly associated with trauma. The Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM 5) requires the following criteria to be met for a diagnosis of PTSD.
A – Experiencing, witnessing or learning about a traumatic event involving a family member or experiencing repeated exposure to traumatic events.
B – Experiencing intrusive symptoms such as recurrent memories, distressing dreams, flashbacks, marked and intense distress to triggers.
C – Avoidance of reminders of the trauma.
D – Negative cognitions and moods associated with the event.
E – Marked alteration in state of arousal and reactivity – self harm, hypervigilance, sleep disturbance, concentration problems.
F – Duration more than one month.
G – Disturbance causing impairment in function.
Beyond Blue and SANE Australia have published statistics showing 45 per cent of Australians will experience a mental illness in their lifetime and 12 per cent will experience PTSD. It should be noted though that not everyone exposed to a traumatic event will develop PTSD. In fact, only 25 per cent of people exposed to a traumatic event will develop PTSD.
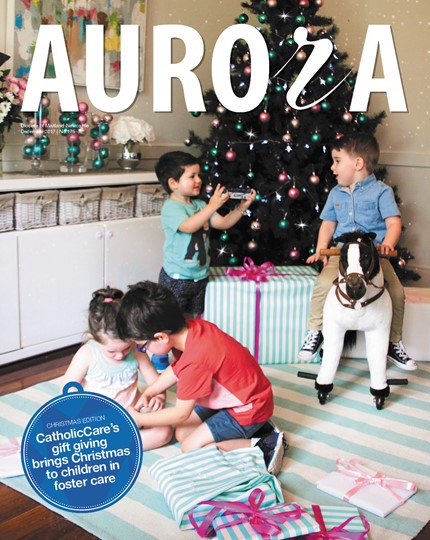
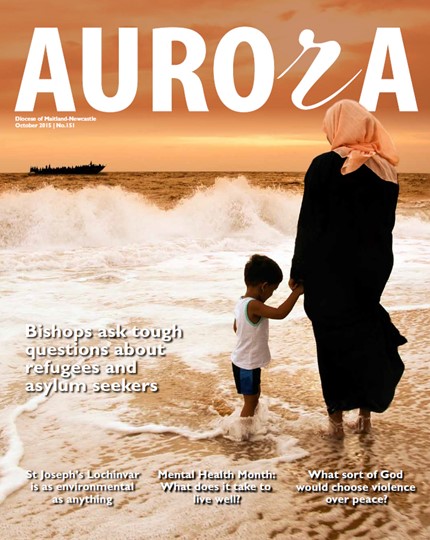
Particular groups in our community such as war veterans, Indigenous Australians, refugees, children in abusive situations or in foster care and emergency workers, can be at greater risk due to their experiences, environment and supports. Everyone experiences trauma differently and your capacity to cope depends on biology, temperament, social supports, and resilience skills developed through past experiences.
Aside from PTSD, trauma has also been associated with:
- anxiety and depression
- substance abuse
- suicidality
- self-mutilation
- aggression and affect regulation
- interpersonal problems – difficulties with relationships
- dysfunctional personality traits
- bingeing and purging
- unsafe and dysfunctional sexual behaviour
- cognitive distortions – extreme hopelessness, low self-esteem
- dissociation – spacing out
- identity disturbance.
The recognition of the impact of trauma has led to the development of a number of trauma-informed therapies. Getting help from a mental health professional early can speed recovery.
Recovery from trauma is not about “deciding to move on” or “willpower”. Seemingly minor stressors constantly trigger the physiological fight or flight response. Trauma-informed care, and supportive and empathetic responses can alleviate levels of distress and support recovery.
There is no doubt trauma is a significant risk factor in developing a mental illness. Continued research is necessary to expand our knowledge and to assist the development of effective treatments. If this article has caused distress or raised your concerns regarding someone close to you, please contact Lifeline on 131114.
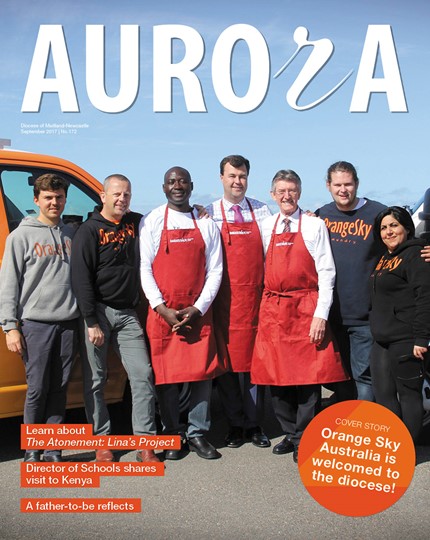
Cheryl Brown is a registered psychologist with CatholicCare Social Services Hunter-Manning.